- Home
- About us
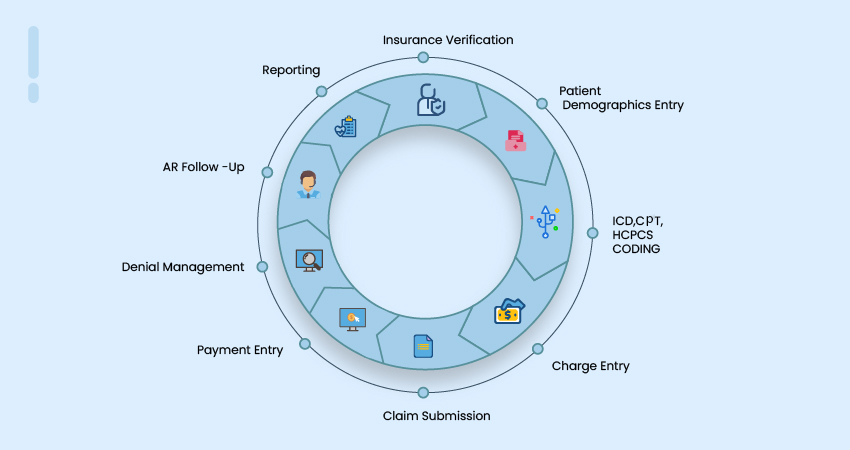
- Services
-
Specialities
-
 Pediatrics Billing Services
Pediatrics Billing Services
-
 Tele Health Billing Services
Tele Health Billing Services
-
 Internal Medicine
Internal Medicine
-
 General Surgery
General Surgery
-
 Pain Management Services
Pain Management Services
-
 Wound care Billing Services
Wound care Billing Services
-
 Urology Billing Services
Urology Billing Services
-
 Skilled Nursing Facilities
Skilled Nursing Facilities
-
 Radiology Billing Services
Radiology Billing Services
-
 Podiatry Billing Services
Podiatry Billing Services
-
 Plastic & Constructive Billing Services
Plastic & Constructive Billing Services
-
 Physical Therapy Billing Services
Physical Therapy Billing Services
-
 Orthopedic Billing Services
Orthopedic Billing Services
-
 Ophthalmology Billing Services
Ophthalmology Billing Services
-
 Oncology Billing Services
Oncology Billing Services
-
 OB/GYN Billing Services
OB/GYN Billing Services
-
 Neurology Billing Services
Neurology Billing Services
-
 Neonatal Billing Services
Neonatal Billing Services
-
 Emergency Billing Services
Emergency Billing Services
-
 Gastroenterology Billing Services
Gastroenterology Billing Services
-
 Dermatology Billing Services
Dermatology Billing Services
-
 Cardiology Billing Services
Cardiology Billing Services
-
 Behavioral & Mental Health Billing Services
Behavioral & Mental Health Billing Services
-
 Anesthesia Billing Services
Anesthesia Billing Services
-
 Ambulatory Surgical Billing
Ambulatory Surgical Billing
-
 Allergy & Immune Billing Services
Allergy & Immune Billing Services
-
- Software Experts
- Careers
- Contact Us